Sub-Phylum: Sarco-mastigophora
Simple protozoa that have no fixed shape. They are classified under the Phylum-.
- The cytoplasm is bounded by a unit membrane and can be differentiated into an outer ectoplasm and an inner endoplasm.
- Pseudopodia are formed by the ectoplasm thrusting out, being followed by the endoplasm flowing in, to produce blunt projections.
- Pseudopodial processes appear and disappear, producing quick changes in the shape of the cell. These are employed for locomotion and engulfment of food by phagocytosis.
- Amoebae may be free-living or parasitic. A few of the free-living amoebae can, on occasion act as human pathogens, producing meningo-encephalitis and other infections.
- Some of them can act as carriers of pathogenic bacteria. The parasitic amoebae inhabit the alimentary canal.
Parasitic Amoebae
Parasitic amoebae belong to the following genera: Genus Species:
1. Entamoeba:
a) Entamoeba histolytica.
b) Entamoeba dispar.
c) Entamoeba coli.
d) Entaomoeba polecki.
e) Entamoeba hartmanni.
f) Entamoeba gingivalis.
2. Endolimax.
a) Endolamix nana.
3. Iodamoeba
a) Iodamoeba butschlii.
4. Dientamoeba.
a) Dientamoeba fragilis.
Entamoeba histolytica
Is an important human pathogen, causing amoebic dysentery as well as hepatic amoebiasis and other extra-intestinal lesions. E.hartmanni is nonpathogenic, though it resembles E. histolytica very closely except for its smaller size and was therefore known as the ‘small race’ of E. histolytica. E.polecki a natural parasite of pigs and monkeys may sometimes infect humans causing diarrhoea.
E. coli is a common commensal in the colon and its importance is that it may be mistaken for E.histolytica. E.gingivalis is present in the mouth, being found in large numbers when the oral hygiene is poor. It has no cystic stage and so the trophozoites depend for transmission on direct oral contact as in kissing, air-borne spread through salivary 9 droplets and fomites such as shared drinking and eating utensils.
It is generally nonpathogenic, though it has been claimed that it contributes to periodontal disease. All the genera of intestinal amoebae other than Entamoeba are nonpathogenic commensals, except D.fragilis, which may occasionally cause chronic, but mild intestinal symptoms. Intestinal amoebae can be differentiated based on their morphological features.
History
- History Entamoeba histolytica was discovered in 1875 by Losch in the dysenteric feces of a patient in St Petersburg, Russia. He also observed it in colonic ulcers at autopsy and produced dysentery in a dog by inoculation through the rectum.
- In 1890, William OsIer reported the case of a young man with dysentery who later died of liver abscess.
- Councilman and Lafleur in 1891 established the pathogenesis of intestinal and hepatic amoebiasis and introduced the terms ‘amoebic dysentery’ and ‘amoebic liver abscess.
Geographical Distribution
E. histolytica is world-wide in prevalence. It is much more common in the tropics than elsewhere, but it has been found wherever sanitation is poor, in all climatic zones, from Alaska (61° N) to the Straits of Magellan (52°S). It has been reported that about 10 per cent of the world’s population and 50 per cent of the inhabitants of some developing countries may be infected with the parasite. The infection is not uncommon even in affluent countries, about 1 per cent of Americans being reported to be infected. While the large majority of the infected are asymptomatic, invasive amoebiasis causes disabling illness in an estimated 50 million persons and death in 50,000 annually, mostly in the tropical belt of Asia. Africa and Latin America. It is the third leading parasitic cause of mortality, after malaria and schistosomiasis. E. histolytica is found in the human colon.
Natural infection also occurs in monkeys, dogs and probably in pigs also but these animals do not appear to be relevant as sources of human infection.
Infection is mostly asymptomatic. It commonly occurs in the lumen of the
colon as a commensal, but sometimes invades the intestinal tissues to become a pathogen.
Morphology
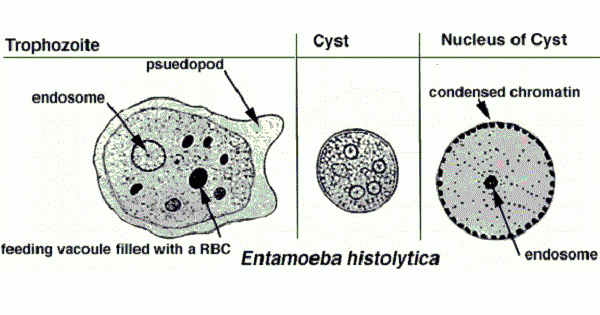
E. histolytica occurs in three forms:
a. Trophozoite.
b. Pre-cystic.
c. Cystic stages.
Trophozoite
- Trophozoite is the vegetative or growing stage of the parasite.
- It is the only form present in tissues.
- It is irregular in shape and varies in size from 12- 60 µm; average being 20 µrn.
- It is large and actively motile in freshly passed dysenteric stool, while smaller in convalescents and carriers.
- The parasite, as it occurs free in the lumen as a commensal is generally smaller in size, about 15-20 µm and has been called the minuta form.
Cytoplasm:
Outer ectoplasm is clear, transparent and refractile. Inner endoplasm is finely granular, having a ground glass appearance. The endoplasm contains nucleus, food vacuoles, erythrocytes, occasionally leukocytes and tissue debris. Pseudopodia : are finger-like projections formed by sudden jerky movements of ectoplasm in one direction, followed by the streaming in of the whole endoplasm.
Typical amoeboid motility is a crawling or gliding movement and not a free swimming one. The direction of movement may be changed suddenly, with another pseudopodium being formed at a different site, when the whole cytoplasm flows in the direction of the new pseudopodium. The cell has to be attached to some surface or particle for it to move.
In culture tubes, the trophozoites may be seen crawling up the side of the glass tube. Pseudopod formation and motility are inhibited at low temperatures. Nucleus is spherical 4- 6 µm in size and contains central karyosome, surrounded by clear halo and anchored to the nuclear membrane by fine radiating fibrils called the Linin network, giving a cartwheel appearance.
The nucleus is not clearly seen in the living trophozoites, but can be clearly demonstrated in preparations stained with iron hematoxylin. Nuclear membrane is lined by a rim of chromatin distributed evenly as small granules.
The trophozoites from acute dysenteric stools often contain phagocytosed erythrocytes. This feature is diagnostic as phagocytosed red cells are not found in any other commensal intestinal amebae.
The trophozoites divide by binary fission in every 8 hours. Trophozoiles survive up to 5 hours at 37°C and are killed by drying, heat and chemical sterilization. Therefore, the infection is not transmitted by trophozoites. Even if live trophozoites from freshly-passed stools are ingested, they are rapidly destroyed in stomach and cannot initiate infection.
Pre-cystic Stage
- Trophozoites undergo encystment in the intestinal lumen.
- Encystment does not occur in the tissues nor in feces outside the body.
- Before encystment, the trophozoite extrudes its food vacuoles and becomes round or oval, about 10- 20 µm in size.
- This is the pre-cystic stage of the parasite. It contains a large glycogen vacuole and two chromatid bars. It then secretes a highly retractile cyst wall around it and becomes cyst.
Cystic Stage
- The cyst is spherical in shape about 10-20 µmin in size.
- The early cyst contains a single nucleus and two other structures a mass of glycogen, and 1- 4 chromatoid bodies or chromatoid bars, which are cigar-shaped.
- The chromatoid bodies are so-called because they stain with hematoxylin , like chromatin.
- As the cyst matures, the glycogen mass and chromidial bars disappear and the nucleus undergoes two successive mitotic divisions to form two and then four nuclei. 1he mature cyst is, thus quadrinucleate.
- The cyst wall is a highly refractile membrane, which makes it highly resistant to gastric juice and unfavorable environmental conditions.
- The nuclei and chromidial bodies can be made out in unstained films, but they appear more prominently in stained preparations. With iron hematoxylin stain, nuclear chromatin and chromaroid bodies appear deep blue or black, while the glycogen mass appears unstained. When stained with iodine, the glycogen mass appears golden brown, the nuclear chromatin and karyosome bright yellow, and the chromatoid bodies appear as clear space, being unstained.
Lif cycle of Entamoeba histolytica
Entamoeba histolytica passes its life cycle only in one host (man). Cysts and trophozoites are typically found in diarrheal stool. Infection by Entamoeba histolytica occurs by ingestion of mature cysts in fecally , contaminated food , and water. Excitation occurs in the small intestine and trophozoites are released, which migrate to the large intestine.
The trophozoites multiply by binary fission and produce cysts, and both stages are passed in the feces. Because of the protection conferred by their walls, the cysts can survive days to weeks in the external environment and are responsible for transmission.
Trophozoites passed in the stool are rapidly destroyed once outside the body, and if ingested would not survive exposure to the gastric environment. The cysts passing in stool of infected individuals. In some patients, the trophozoites invade the intestinal mucosa or, through the bloodstream, extraintestinal sites such as the liver, brain, and lungs, with resultant pathologic manifestations.
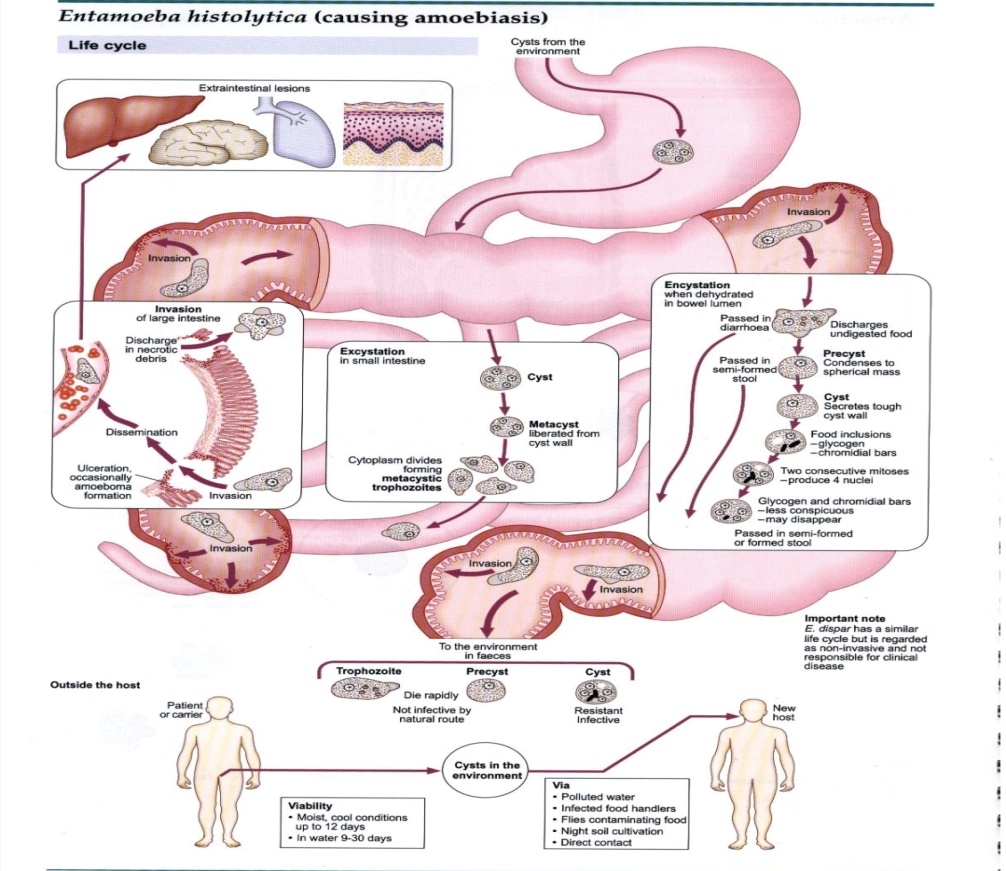
Infective Form
Mature quadrinucleate cyst passed in feces of convalescents and carriers. The cysts can remain viable under moist conditions for about 10 days.
Mode of Transmission
Man acquires infection by swallowing food and water contaminated with cysts.
Excystation: Is hapened when the cyst reaches cecum or lower part of the
ileum, due to the alkaline medium, the cyst wall is damaged by trypsin.
Metacyst mean the cytoplasm gets detached from the cyst wall and ameboid
movements appear causing a tear in the cyst wall, through which quadrinucleate ameba is liberated.
Meta-cystic Trophozoites mean the nuclei in the metacyst immediately
undergo division to form eight nuclei, each of which gets surrounded by its
own cytoplasm to become eight small amebulae or meta-cystic trophozoites.
Pathogenesis and Clinical Features
E. histolytica causes intestinal and extraintestinal amebiasis. Incubation period is highly variable. On an average, it ranges from 4 days to 4 months.
Amebiasis can present in different forms and degree of severity, depending on the organ affected and the extent of damage caused.
Intestinal Amoebiasis
The lumen-dwelling amebae do not cause any illness. They cause disease only when they invade the intestinal tissues. This happens only in about 10% of cases of infection, the remaining 90% being.
Asymptomatic.
Not all strains of E. hislolylica are pathogenic or invasive. Differentiation between pathogenic and nonpathogenic strains can be made by susceptibility to complement mediated lysis and phagocytic activity or by the use of genetic markers or monoclonal antibodies and zymodeme analysis.
Amebic ulcer
Is the typical lesion seen in intestinal amebiasis.The ulcers are multiple and are confined to the colon, being most numerous in the cecum and next in the sigmoido-rectal region. The intervening mucous membrane between the ulcers remains healthy. Ulcers appear initially on the mucosa as raised nodules with pouting edges measuring pinhead to l inch. They later break down discharging brownish necrotic material containing large numbers of trophozoites.
The typical amebic ulcer is flask-shaped in cross section, with mouth and neck being narrow and base large and rounded. Multiple ulcers may coalesce to form large necrotic lesions with ragged and undermined edges and are covered with brownish slough.
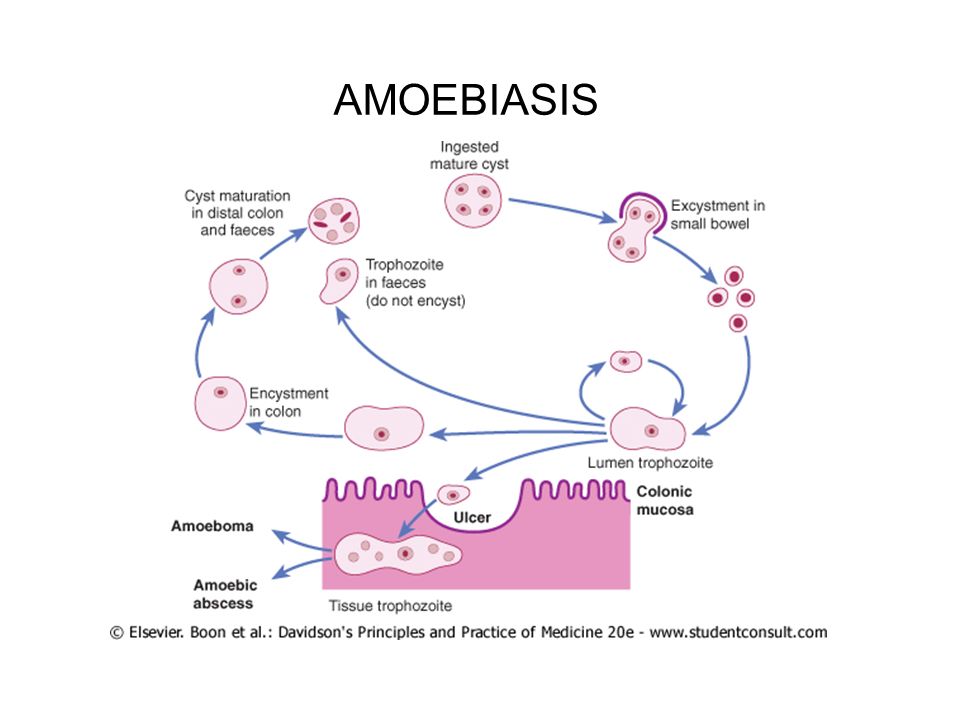
Ameboma
Occasionally, a granulomatous pseudo-tumoral growth may develop on the intestinal wall by rapid invasion from a chronic ulcer. This amebic granuloma or ameboma may be mistaken for are malignant tumor. Amebomas are most frequent at cecum and recto-sigmoid junction.
Laboratory diagnosis of Entamoeba histolytica
Stool examination: Bloody and\or mucoid stool sample to see trophozoite and cyst stages by normal saline and Lugol's iodine direct smear respectively.
The sample (stool) should be collected into a wide mouth container and examined without delay, and should be inspected via: Macroscopy and Microscopy.
Macroscopy:
The stool is characterized by :
Foul-smelling, copious, semiliquid, brownish -black in color, intermingled with blood and mucus, and it does not adhere to the container.
Microscopy
Saline preparation:
1. The cellular exudate is scanty and consists of only the nuclear masses
(pyknotic bodies) of a few pus cells, epithelial cells and macrophages.
2. The RBCs are in clumps and yellow or brown -red in color.
3. Charcot-Leyden crystals are often present. These are diamond-shaped,
clear and refractile crystals.
4. Actively motile trophozoites throwing pseudopodia can be demonstrated
in freshly-passed stool. Presence of ingested RBCs clinches the identity of E. hislolytica. Nucleus is not visible but a faint outline may be detected.
5.Cyst has a smooth and thin cell wall and contains round refractile chromatoid bars. Glycogen mass is not visible.
Iodine preparation:
For the demonstration of cysts or dead trophozoites, stained preparations may be required for the study of the nuclear character. Iodine-stained preparation is commonly employed for this purpose. The trophozoite of E. histolytica stains yellow to light brown. The nucleus is clearly visible witl1 a central karyosome. The cytoplasm of the cystic stage shows a smooth and hyaline appearance. Nuclear chromatin and karyosome appear bright yellow. Glycogen masses stain golden brown and chromatoid bars are not stained.
The trichrome stain is useful to demonstrate intracellular features of both trophozoites and cysts. Since the excretion of cysts in the stool is often imminent, at least three consecutive samples should be examined. Mucosal scrapings: Scraping obtained by sigmoidoscopy is often contributory. The examination method includes a direct wet mount and iron hematoxylin and immunofluorescent staining with anti-E.hislolytica antibodies.
Stool culture
Stool culture is a more sensitive method in diagnosing chronic and asymptomatic intestinal amebiasis.
The culture of stools gives higher positivity for E. histolytica as compared to direct examination.
Media used for stool culture include to diagnosis the E. histolytica:
1.Boeck and Drbohlav's biphasic medium.
2. NIH polygenic medium
3. Craig's medium
4. Nelson's medium
5. Robinson's medium
6. and Balamuth's medium.
Serological -diagnosis
Serological tests : become positive only in invasive amebiasis.
Antibody detection
Amebic antibodies appear in serum only in the late stages of intestinal amebiasis. Tests for antibodies in scrum help in the diagnosis of mainly extraintestinal infections. Serological tests include:
- Indirect hem-agglutination assay (IHA)
- Indirect fluorescent antibody (IFA)
- Enzyme-linked immunosorbent assay (ELISA)
- Counter-current immunoelectrophoresis (CIEP)
- Latex agglutination tests.
Serum with an antibody titer of 1:256 or more by IHA and 1:200 by IFA are considered to be significant.
Amebic antigen detection
Amebic antigen in serum are detected only in patients with active infections and disappears after clinical cure. Antigen like Lipophosphoglycan (LPG) amebic lectin, serine-richE. histolytica protein (SREHP) are detected using monoclonal antibodies by ELISA.
Molecular diagnosis
Recently, deoxyribonucleic acid (DNA) probes and radioimmunoassay have been used to detect E. histolytica in the stool. It is a rapid and specific method.
Treatment
Both luminal and tissue amebicides: Metronidazole and related compounds like tinidazole and omimidazole act on both sites and are the drug of choice for treating amebic colitis and amebic liver abscess.

